Churches have been urged to step into the gap left by overstretched mental health services during an online mental health summit hosted by NAYBA Australia, a network helping churches to transform neighbourhoods.
Gavin Brown, Director and Senior Clinical Psychologist, at Rapha Health, told the summit that mental health was the church’s “Mars Hill moment” – referring to the apostle Paul’s engagement with the people of Athens in Acts 17 – and the similar opportunity to begin engaging with the wider community.
He said mental health services across Australia were “completely overwhelmed” and in many places there weren’t any psychologists to refer people to.
“There’s huge workforce issues. There’s a huge gap there. And we can step into that, and this is a place where, if we start to say, ‘This is really serious for us, we want to be able to help,’ people are not going to turn us away,” he said.
“There are lots of areas, unfortunately, in our society where probably the church across the board struggles to be relevant. Here is our Mars Hill. This is what we can actually do. So I just want to encourage you in that.”
“All the stuff that’s on our news – it’s all mental health.” – Gavin Brown
Brown was one of a panel of church leaders, mental health practitioners, lived-experience advisers, and theologians who led over 100 participants from across the country in a conversation about how churches can respond to Australia’s mental health crisis. While none suggested churches could replace professional psychological services, they emphasised that churches should offer a community of friendship to assist people struggling with mental health.
“Mental health is where the community is at,” he said. “You know, all of the stuff that we’re talking about, all the stuff that’s on our news – it’s all mental health. Our housing crisis in Australia is a mental health issue. Cost of living pressures is a mental health issue. The floods in Victoria are a mental health issue.
“It’s all mental health, and we have this fantastic opportunity as the church to really engage in this space, to not see it as the domain of specialists or people that are specifically trained, but that it’s all of us.”
“As followers of Jesus we should actually be better at therapeutic relationships than anyone because of who our model is.” – Gavin Brown
Brown said one reason churches had a responsibility to engage in this space was that it provided a community of friends.
“So many of our mental health diagnoses either have at their core or as a consequence, a relational problem, that they either originate from a relational problem or that a consequence of that illness is a relational issue,” he explained.
“As I said, reading the Bible and praying is great thing to do, but we have a relational God. And it strikes me that a relational God does not actually seek to heal people outside of relationships and that’s why what we do as the church is so, so important.”
He said there were over 400 psychological therapies that a person could receive from a psychologist, but research shows that the treatment largely doesn’t affect the outcome.
“The one thing that predicts the effectiveness of outcomes and psychological treatment is the quality of the therapeutic relationship, and studies over and over again reiterate that, and I would argue that as followers of Jesus we should actually be better at therapeutic relationships than anyone because of who our model is. That’s our calling.”
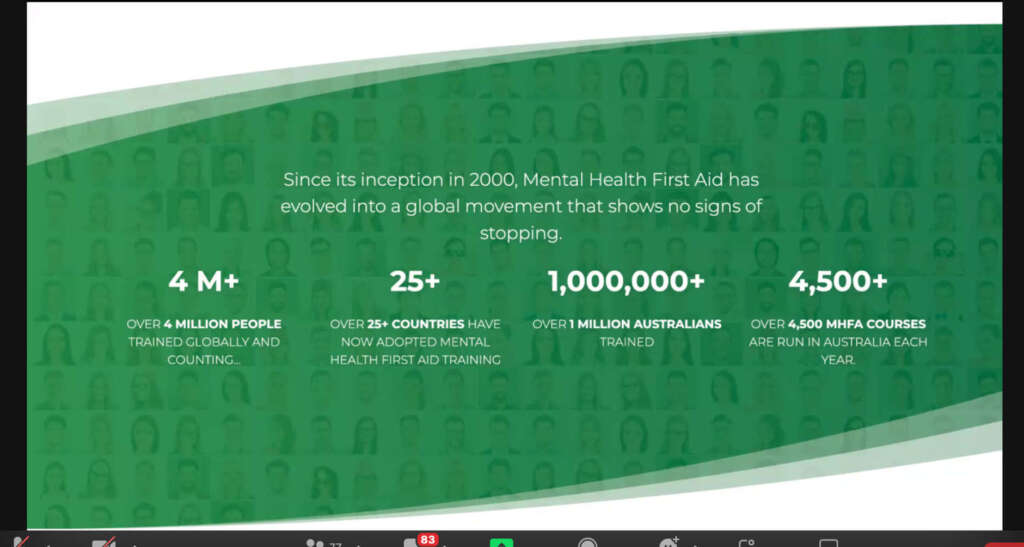 Under Brown’s leadership, as a clinical psychologist and former chaplain, Rapha Health has become a leading provider of the Mental Health First Aid program, which delivers in-house training for a range of businesses as well as church and faith communities. Started in Australia in 1997, this two-day workshop has now gone global. It seeks to teach ordinary people about common mental health issues and how to respond to them in the initial stages.
Under Brown’s leadership, as a clinical psychologist and former chaplain, Rapha Health has become a leading provider of the Mental Health First Aid program, which delivers in-house training for a range of businesses as well as church and faith communities. Started in Australia in 1997, this two-day workshop has now gone global. It seeks to teach ordinary people about common mental health issues and how to respond to them in the initial stages.
“One of the things that Mental Health First Aid has is what’s called a recognised workplace program. So there are workplaces that can go, ‘Yep, this is really important to us. We want to get a certain percentage of our people trained in mental health and have them aware and able to intervene.’ And when they do that, Mental Health First Aid has a list of all the workplaces that have committed. I looked at that long list the other day, and sadly, as far as I can see, there is not one single church on that list.”
“And that’s obviously why these conversations are so important. I think one of the saddest things in our society, as a Christian, is that really the psychologist office has become the new confessional.
“That’s what we are. We have a safe space now where people will come and say things that they wouldn’t dream of saying to anyone else, and I don’t want them to come here and say [that]. I want them to be able to go to the church and say that because that I believe is a really crucial part of our role.”
Fiona Hall, Director of Ministries at Crossway Baptist Church, said she would seek to get her church on that list of recognised workplaces because it already working to have every single member of its staff trained in Mental Health First Aid.
She said Crossway Baptist had set up Crossway Life Care about 18 years ago as a counselling centre with counsellors and psychologists who help people who are unable to afford professional help. But since the extensive lockdowns from the pandemic, demand for such counselling had shot up, especially in Victoria, with a host of new clients.
“What we’ve seen is they’re not the same people as were coming before the pandemic. So we’ve got a wider breadth of society who are now looking for mental health support,” she said.
“[So] in the same way that we have First Aid for physical injuries, we decided that what we really needed to do is get on board with the Mental Health First Aid. We trained one of our counsellors as a mental health first aid trainer, and we’ve been putting through as many staff and team as possible so that they can all be trained in mental health.”
In a discussion of resources available to help train churches in mental health intervention, host of the summit, Nic Mackay mentioned Sanctuary Mental Health Ministries and EDIFY, both of which have been accredited as NAYBA Recognised Projects.
Daniel Whitehead, CEO of Sanctuary, dialled into the Summit from Canada. He explained that it’s a course similar to the Alpha course in that it’s a high-quality resource that anyone, anywhere, can pick up and facilitate.

A Sanctuary course small group
Whitehead created the course along with Dr John Swinton, Professor in Practical Theology and Pastoral Care at the University of Aberdeen, who also addressed the summit.
“We launched it four years ago, and in the last four years, it’s been downloaded in 60 countries. And over 200,000 people have been through it,” Whitehead said.
“A Sanctuary course is an eight-session course that looks at core subjects, core important things that we have to address before we can really have a good conversation about mental health. What it does is it creates this safe space for small groups to share their own experiences and to get a shared framework and shared language from which a culture of mental health ministry can be built.”
Whitehead said all of Sanctuary’s resources were free. While the Sanctuary courses were the flagship resource, they were also working on ten new resources including a youth course, with much of the filming in Australia. They are also creating an album of music with the Porters Gate – a sacred ecumenical arts collective – to be called Sanctuary Songs, which will provide churches with worship music that broaches the subject of mental health. Sanctuary was also working with the British Bible Society to create a mental health and wellbeing Bible, which will have an international release, along with a podcast around spiritual trauma. These would all be available within the next 15 months.
Nic Mackay then provided an overview of EDIFY, a program that equips local churches with counselling and training resources. Developed in South Africa, it offers training at three levels – self-care, community care, and pastoral care.
“What I love about EDIFY is that it recognises that there’s only a very small percentage of people dealing with issues of mental ill health who require professional care,” he said.
“A key part of the role of the church can actually be intervening at the earlier points in the journey as people begin to experience mental ill health. And if we can make sure that we’re not only caring for ourselves, and our faith community, but also able to offer pastoral care in the form of counselling servicesto those in the wider community, we can actually help to prevent the numbers of people who then require the level of professional care.”
Email This Story
Why not send this to a friend?


