When Kate steps on to the floor of the newly-created COVID-19 ward in the Sydney hospital where she works, it’s a bit like walking into a war zone.
“The most helpful thing I’ve found to help me through this – although not talking about the spiritual side of things – is to think of this like wartime,” says Kate, a respiratory specialist.
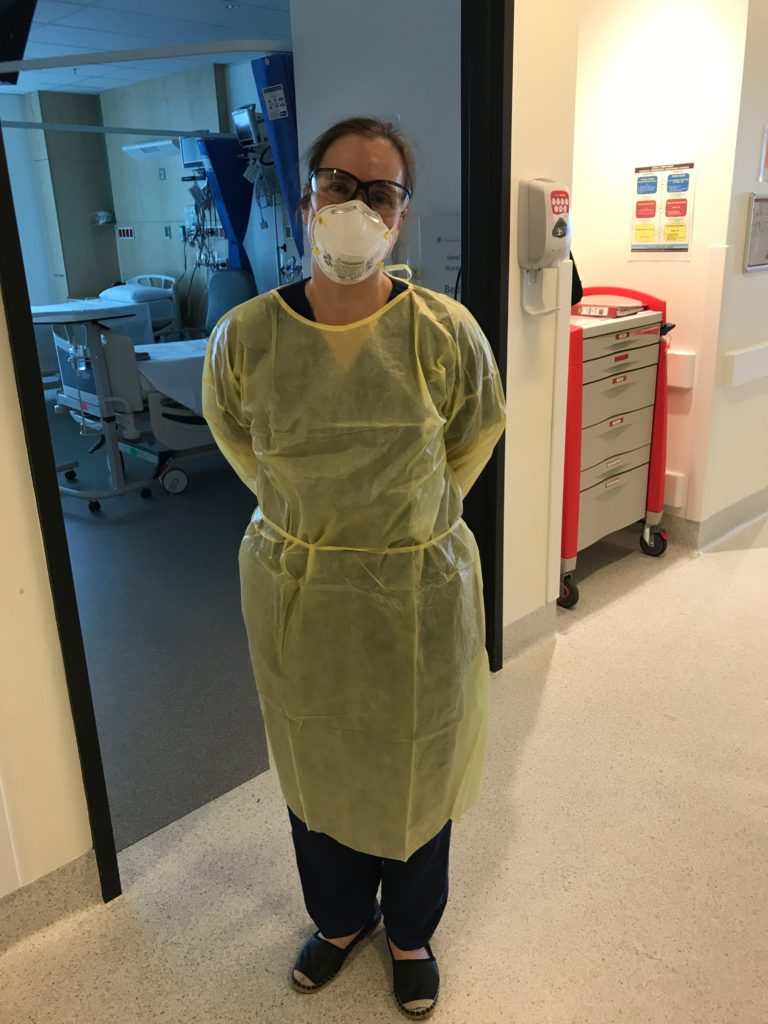
“I find great encouragement by remembering people who had to fight in the wars and send their children off to war – the idea that you do your bit for your country. That actually gives me courage to put my hand up, to get into my PPE [personal protective equipment] and get on that ward.
“We’ve all got to do our bit … my bit is to go on the ward.” – Kate
“Because we’ve all got to do our bit. There’s not a lot of other people who are trained as respiratory physicians. Other people can do their bit by staying home and washing their hands, but my bit is to go on the ward.”
On the COVID-19 ward
As a lung doctor, Kate divides her days between her practice, a tuberculosis clinic and the hospital. However, since COVID-19 struck, more and more of her time is being devoted to the hospital at it braces for the likely onslaught of coronavirus patients.
Kate is at the forefront of her hospital’s COVID-19 committee, and so her last few weeks have been a blur of non-stop phone calls, messages, webinars, video conferences, training sessions and digesting the ever-changing tide of information from Australia and overseas about this dreaded disease.
“It’s quite tricky to keep up to date – you can’t print out a protocol because by the afternoon it’s outdated. And like everybody, I think our IT skills have had to grow exponentially,” she explains.
“There’s no guide book about this … It’s a disease that we’re still learning about.” – Kate
From the time she wakes – often at 4am when her mind starts ticking over – to the time she goes to bed, Kate’s time is consumed by COVID-19 – even on her “days off”.
“I have no mental break because there’s no guide book about this … It’s a disease that we’re still learning about. I’ve been through medical school and then my specialty training where you learn all about diseases – and you know all about them – whereas I’ve never managed this one before.”
Then there’s the time pressure for new, best-practice hospital procedures to be implemented and for all staff to be trained.
“Two weeks ago, Germany had around about the same number of cases as we have now, and now they’ve got 40,000. So we just don’t know when it will really ramp up, but I would imagine in the next couple of weeks,” Kate predicts.
“And so it really feels like there’s this deadline and this pressure to get things done, like implement protocols, so that everyone is kept safe.
“I think that’s what Italy showed us, that if you don’t have that bedded down, and you don’t take care of your staff, it becomes out of control.”
“I’ve never thought about death as much as I have in the last two weeks.” – Kate
Of course, despite the best preparations, there’s still a fear that Kate might catch COVID-19.
She admits: “In the background, there’s always the thought that I might catch this. I’ve never thought about death as much as I have in the last two weeks.”
Kate also admits that keeping her awake at night are decisions about prioritising patients, as well as the need to keep hospital staff safe. Although, as a Christian, she does have a supernatural confidence about the world’s health crisis.
“At this time, what people trust in and put their confidence in has all been stripped away – their jobs, what they look like, sport, individual freedoms. As Christians, not just as doctors, this shouldn’t shake us too much because our confidence is not in the things of this world, it’s in God …”
“This is a trial, but good stuff can come out of it. And I have to trust God. I might get sick, but it will be according to God’s plan.”
Kate
In the GP clinic
Kate’s husband Pete, a GP, has also spent the past few weeks in his Sydney clinic implementing new protocols to ensure staff and patients are kept safe from the virus. These protocols – on the advice of the Royal Australian College of General Practitioners (RACGP) and NSW Health – have evolved to locking the front door and posting a sign with the clinic’s phone number to ensure that patients do, in fact, call before entering.
As well as phone consultations, Pete has spent many hours on the phone just reassuring patients.
“Some people are just terrified and they’ve rung eight times or they’ve tried three different doctors and gone to three different surgeries to get a test, and they can’t get a test,” he says.
“We do have a responsibility to the whole healthcare system not to send every man, woman and child for a test.” – Pete
While Pete is sending some people for COVID-19 testing, he adds, “we do have a responsibility to the whole healthcare system not to send every man, woman and child for a test and overrun the testing centres.”
The practice has divided its day into chunks in order to separate well patients who are coming in for routine visits, like vaccinations, and those who are sick with respiratory symptoms but don’t meet the COVID testing criteria.
On top of this, surfaces must be disinfected after every patient. Face-washers used for hand and surface cleaning (because paper towel is no longer available) must be hot washed. The receptionists in Pete’s clinic now work from behind a Perspex screen – “they’re very vulnerable, more so than us really,” he says.
But not every GP clinic is so well prepared for COVID-19.
“Some surgeries we’ve heard of don’t have any separation of sick and well patients. They don’t have any guidelines – people who have just come in off planes for testing sit in a waiting room with elderly patients who have emphysema, which is negligent. That’s just terrible,” says Pete.
He also notes how hard this period of adjustment is for older GPs lacking computer skills, and for clinics that have doctors who are elderly or who have health conditions themselves.
“One of my colleagues, who has diabetes, should avoid contact with patients where possible. So at least one of our doctors is now working entirely from home, so that puts pressure on the rest of the team.”
Seeing the positives
For Kate and Pete, who have three school-aged children, there is the added pressure of homeschooling. While Pete has cut his hours down by half, there is still a need for their kids to attend school when he has to work in the clinic.
“There’s a whole other layer of complexity around how we are going to manage once the school holidays hit,” says Kate – and even more complexity if or when schools do close in NSW for a longer period.
However, she adds quickly: “We’re very mindful of the fact that many people out there don’t have any work at all, so we’re lucky from that point of view.”
“You do feel like you’re part of this massive team across the world who’s trying to help each other out.” – Kate
Another positive that Kate points out is the way in which health professionals in her own hospital and across the world are coming together to work collaboratively.
Her hospital’s COVID-19 committee – like that in other major hospitals – draws together professionals in each specialty. These include infectious diseases, cardiology, respiratory, general medicine, intensive care, anaesthetics and the emergency department – as well as those in hospital management.
“I have to say, I’m in no way alone. My team of doctors at the hospital are incredible. And we’re all really pulling together. It’s just amazing how well we’re working together,” says Kate.
She is also part of a newly-created online critical care group, with hundreds of other Australian doctors, created to share information about COVID-19. Much of this information comes from overseas, and it has valuable lessons for Australian doctors.
“China has published handbooks about how to manage things, and they’re trying to get everything out as quickly as possible so that people can use it.”
“China did a global webinar where a million people logged in, and Italian doctors are also doing webinars.
“You do feel like you’re part of this massive team across the world who’s trying to help each other out,” says Kate.
“Pray that Christian healthcare workers will show true peace and good leadership in a healthcare storm.” – Pete
This information will become critical for Australian hospitals as the number of infections grow and doctors have to make difficult decisions about how best to use limited resources.
“That’s where we’ll need the collaborative international resources from China, from Italy and from the UK about, for example, what sort of person doesn’t do well in intensive care, so that it’s not based on our best guess,” explains Kate.
“We can know that someone like this will die, so let’s make them comfortable and let’s not take up a ventilator – but based on science, not based on best guess.”
Pete adds: “If it gets as bad as other countries, then healthcare workers will be tested to their limits.”
“I’ve heard at some hospitals that some staff members are already scared – they’re terrified of what’s to come.”
He continues on a note of reaching out to higher help: “Pray that Christian healthcare workers will show true peace and good leadership in a healthcare storm – that we would give comfort to those around us and that will be evidence that our trust is in something that is not seen but which is far greater.
“That [even] in the fear, which is real, we trust in an all-powerful God.”
Pray
Some prayer points to help
Kate and Pete provide the following prayer points for healthcare workers in Australia and around the world:
Pray for the safety of healthcare workers – that they will be protected being infected with COVID-19
Pray that healthcare workers will be courageous – for the community, for the healthcare system and for the Australian effort against this disease
Pray for the decision makers in hospitals – that they would have godly wisdom, love and compassion
Pray for rapid decision making from governments in terms of providing equipment and support to healthcare workers
Pray that Christian healthcare workers will show true peace and good leadership in a “healthcare storm” – that they would give comfort to those around them and that it will be evident that their trust is “in something that is not seen but which is far greater.”




